How Ivoclean Works
How Ivoclean Works
Lee Ann Brady, DMD
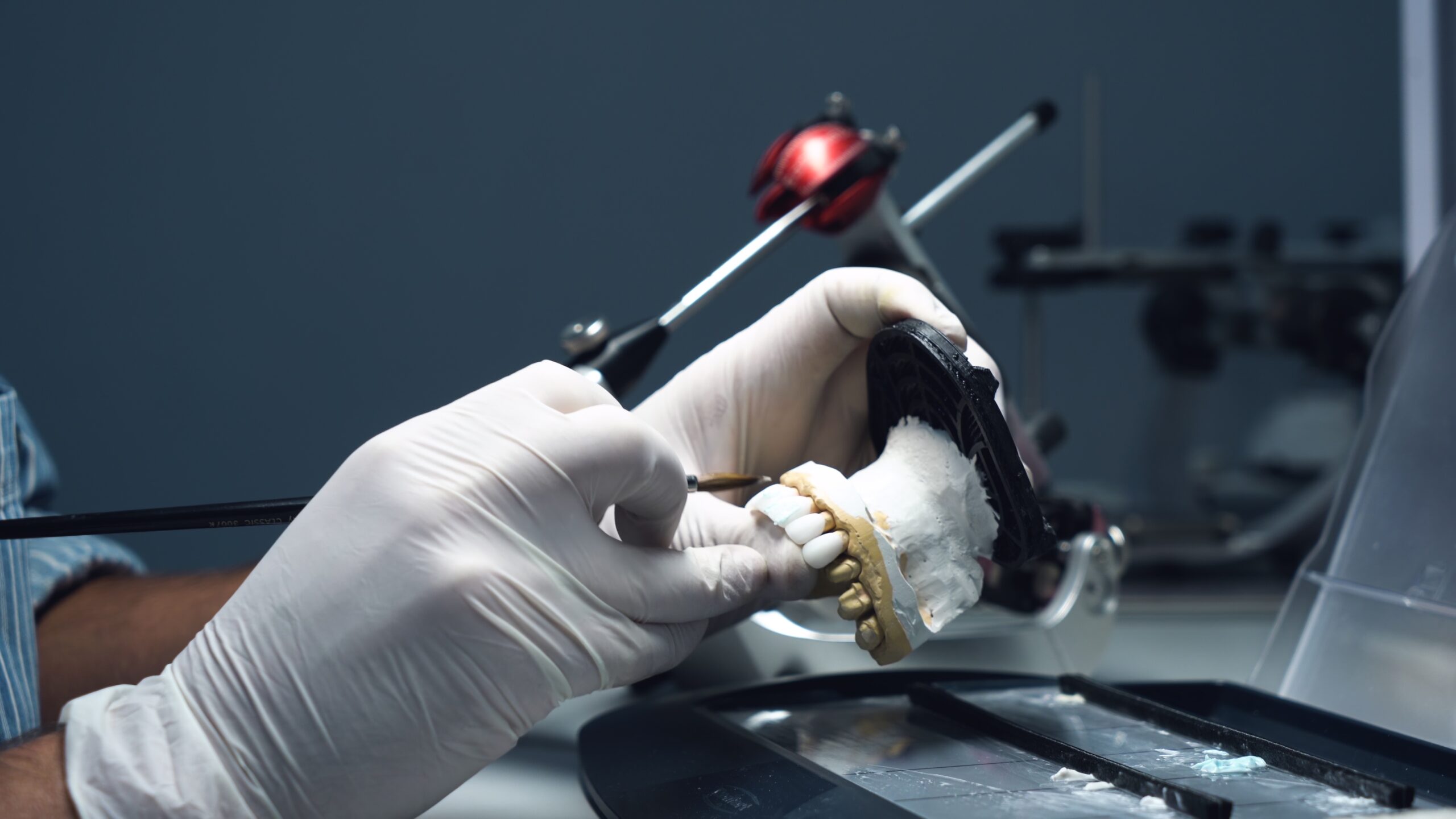
Saliva on the inside of restoration surfaces greatly reduces the bond strength between the porcelain and the cement but during the intraoral try-in process, it is inevitable that there will be saliva contamination.
Most dentists I know use Ivoclean from Ivoclar to clean their indirect restorations after try-in. It is an incredible material for removing saliva and other contaminants that the restoration is exposed to during the intraoral try-in process.
We trust Ivoclean to fully remove resin or traditional cements, as well as saliva and red blood cells to produce a super pristine surface.
Did you ever wonder how Ivoclean works to get rid of saliva and all the other debris that gets on the inside of a ceramic restoration or metal base?
Intraoral contaminants contain lots of phosphates. Ivoclean contains suspended zirconia particles that have an affinity for phosphates. The zirconia particles pull towards them the phosphate-laden particles, so when you rinse off the Ivoclean, the intraoral debris is rinsed away leaving a clean surface.
Note: We don’t want to expose zirconia restorations to something that contains phosphates or includes phosphoric on the label because there is a strong attraction at an elemental level between zirconia and phosphate particles. To neutralize the ionic bond between saliva phosphates and zirconia, we need an alkaline solution such as potassium hydroxide (KOH). This is the active ingredient in products such as ZirClean from BISCO.
Related Course
Clear Aligner Therapy: Enhance Restorative Outcomes & Patient Health
DATE: May 23 2024 @ 8:00 pm - May 23 2024 @ 9:00 pmLocation: Online
CE HOURS: 1
Course Description: Review the digital workflow as part of the comprehensive exam and health screening during periodic exams. We will discuss the benefits of clear aligner therapy prior to restorative care. Also the…
Learn More>