I’m a restorative dentist with a passion for occlusion. I’m a firm believer that our patients deserve our best efforts to eliminate deleterious stomatognathic forces that impact comfort, function, smile aesthetics, and whole health. So, I encourage all dentists to wrap their minds around the area of “occlusion” and become immersed in hands-on, mentored courses to better diagnose and treat their patients.
In teaching at The Pankey Institute, I often hear clinicians view occlusion as a great, big mystery, and yes, sometimes misery. At each stage of my developing interest, knowledge, and skill, I have found my passion for occlusion grows and results in better clinical management and outcomes with my patients. When a well-planned full mouth equilibration is completed, the patient’s elation over how their “bite feels” cannot be matched in dentistry.
So, What’s So Hard About Occlusion?
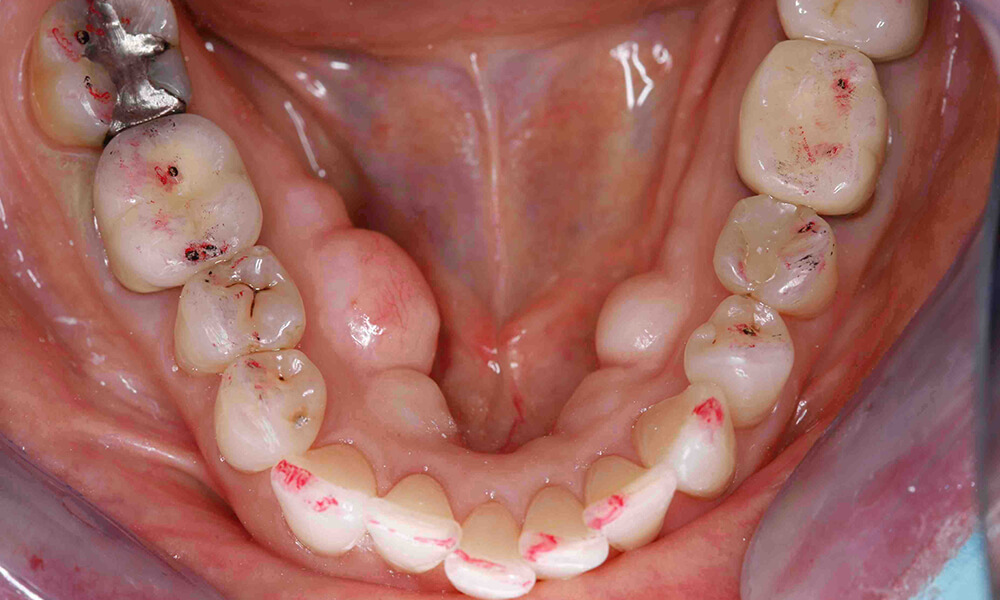
L. D. Pankey was said to say that occlusion is getting the posterior teeth to touch all at the same time with light contact, and when you bite firmly, neither the joint nor the teeth should move. In addition, when you move your jaw left, right, or forward ONLY the front teeth should touch. He would chuckle and say, “So what’s so hard about Occlusion?”
Another way to think about it is that the jaw operates like a tricycle; the two little wheels are the joints, and the big wheel is the front teeth. To have a smooth ride, the steering mechanism and the joints shouldn’t have any notches in them!
Where My Journey in Occlusion Began
Although occlusion was integral to my dental school education, it really wasn’t until I went to the Pankey Institute that my real journey in occlusion began. While I went through the Continuums at the Institute, I joined several technical study clubs. Under the direction and encouragement of Drs. Richard A. Green and Herb Blumenthal, I explored many facets of Occlusal Therapy and TMD.
My View Today
Today I see the occlusion/bite as a potentially significant factor in the balance and harmony of the patient’s whole health. Integrative dental health involves looking for the impact of “other” on the entire body, as my colleague Dr. John Droter states it. The airway, myofunctional impact, and the body’s posture and structural integrity may influence how the teeth come together. If the teeth are chipping, breaking, or intermittently sensitive, it could be the bite. Headaches can be directly associated with the bite. Establishing occlusal harmony – getting rid of “any notches” in the steering mechanism and joints, is a process best tested with a finely balanced bite appliance.
Today I see occlusion as a case-by-case riddle. Every patient is an individual, and their occlusal management is customized accordingly. When solving each patient’s riddle, I’m trying to see how harmony can be re-established in the system of joints, muscles, and teeth. I utilize a bite appliance as a mechanism to test out an occlusal scheme for the patient. Once harmony is achieved, the challenge is to wax and plan the case to mirror the harmony established on the appliance.
For each patient, I’m also trying to figure out how the patient responds to appliance therapy to determine the best treatment modalities or modality. Is the treatment limited to the dentition or is intervention in the joint appropriate?
Either way, my governing philosophy is to make the fewest changes to the dentition while producing the best result for the patient. For some patients, this could be full mouth rehabilitation and for others simply equilibration and/or orthodontics.
Beyond the Teeth and Joints
We are a closed loop from head to toe, and the influence of the stomatognathic system on the “whole” body is best not ignored. Research shows that the teeth, jaws, and tissue affect different areas of the body, impacting for example head, neck, heart, pulmonary, and gastrointestinal health.
In establishing harmony between the dentition and joints, we are calming the musculature. In my mind’s eye, I see occlusal harmony calming the whole system.
Dentists who participate in E1 invariably say it is both an inspiring and practical course, and they want to come back for E2.
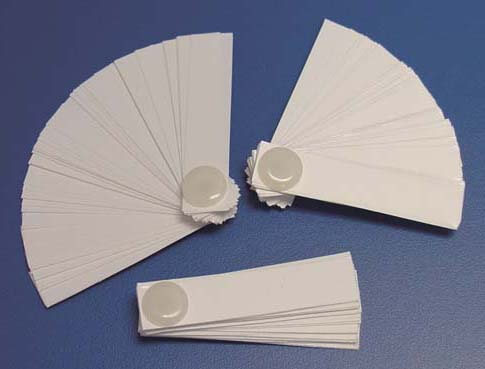
In E1, you will receive enormous encouragement to stay inquisitive and engaged in learning. You will gain insights that impact all aspects of dental practice, and when it comes to occlusion, you will be immersed in a combination of presentations and hands-on exercises coached by experts. The Pankey Institute excels at removing “the misery” out of occlusion by coaching you as you perform exams on colleagues, do diagnostic work ups, and practice making occlusal changes with models, wax, and appliances in the Pankey lab.
“Patients, who seek your care, want the best care you can give them. I believe the Pankey Essentials continuum is one of the best continuums on the planet to learn how to solve occlusal puzzles. Without this “essential” development, we are not the best physicians we can be.” –Kevin Muench DMD