By Laura S. Harkin, DMD
My dad and I were enjoying our favorite lunch spot years ago when he turned to me and said, “Laura, isn’t it amazing? There’s an incredible sense of trust that our patients have in us. Sometimes, we give our best recommendation for treatment, and it is declined as if it weren’t important or a priority. I’ve recognized that, more often than not, our patients eventually choose to move forward, proving that it was more a matter of timing and circumstance than lack of value.”
Trust is the cornerstone of our practice. It was transferred from patients to Grandpa to Dad and to me. I do believe that every morsel is earned through guidance, thoughtfulness, and skill. Trust is an entity that requires constant nurturing. In private practice, one should recognize that a doctor’s trust in their patient is equally as important as a patient’s trust in their provider. With synergy there’s the opportunity for optimal health. Even as a child, I had a very clear understanding of the care my dad had for his patients. This feeling is innate and deeply imbedded in me. I imagine that he felt the same.
I don’t consider myself “a writer,” but I’ve always enjoyed the art of letter writing. I grew up writing frequently to my grandparents and friends and always loved picking out stationary that reflected my personality. Recently, I reread the letters that my grandfather typed on his old typewriter and my oldest brother scribbled on his Grateful Dead CD inserts – crafted just for me. It seems fitting then that I enjoy writing personalized letters to my patients. In fact, I’m pretty sure I salvaged my mental health during COVID by writing “updates” to my patients during months of closure. I digress.
The letters that I write to my patients are most often in reference to comprehensive treatment. They provide a bird’s eye glimpse of our most recent findings, diagnoses, and treatment recommendations. My older patients, especially, appreciate my thoroughness, organization, and systematic approach to recommended treatment. These letters certainly aren’t handwritten, but the hard copy renders a sense of care that’s transferred from my hands to theirs. We must remember that individuals comprehend and retain information differently. The one-on-one, verbal, treatment consultation can become lost in the shuffle of everyday. Add dental language and complicated procedures to the mix, and that’s simply a recipe for confusion.
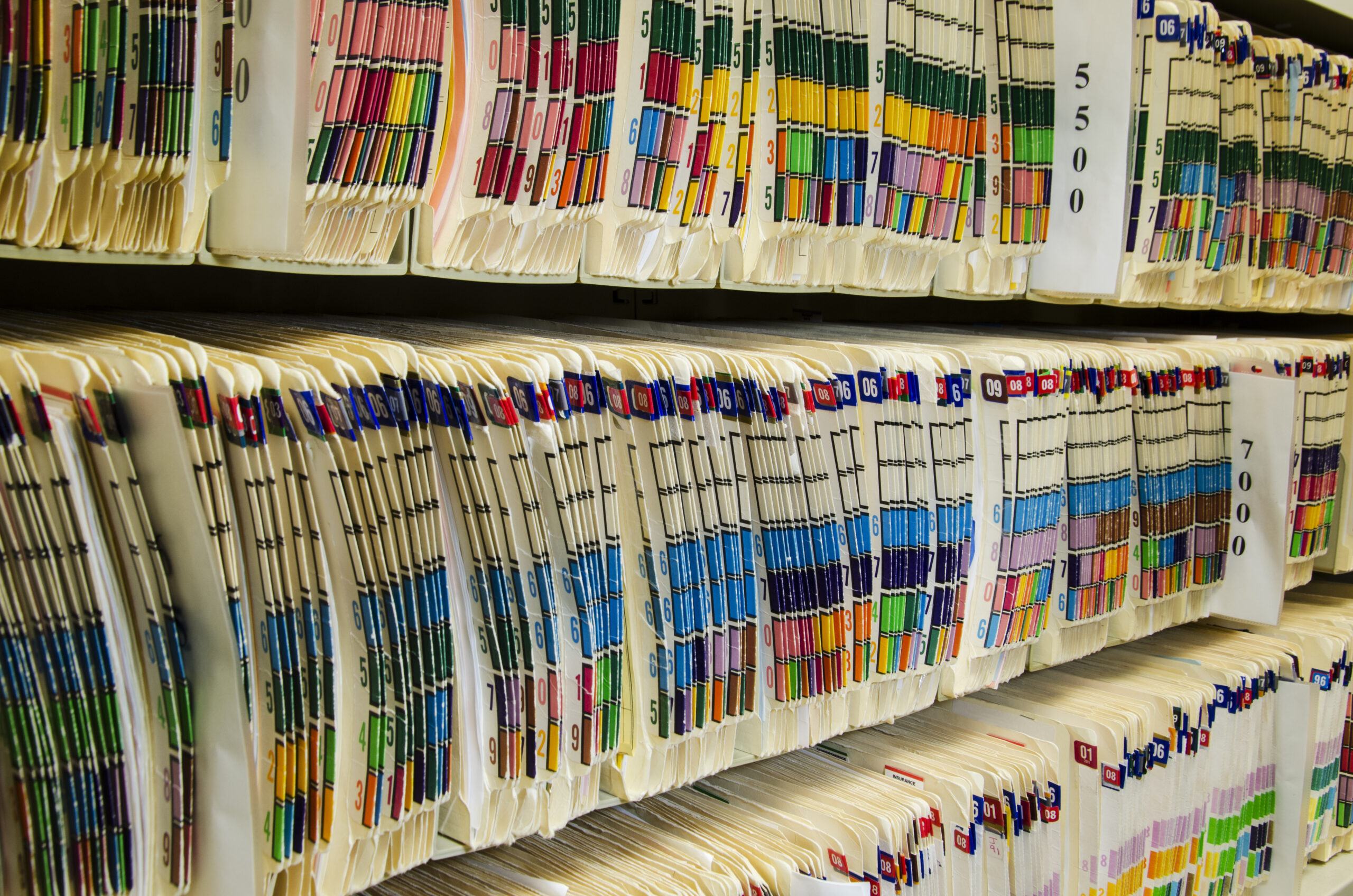
Whenever I present complex treatment to a patient, I write a letter in everyday language to support our conversation. It’s stored in their digital chart as part of their dental record. In my first paragraph, I state my patient’s chief complaint. A summary of clinical findings followed by bullet point. Next, I provide my best treatment recommendation, an appointment sequence, and the financial investment. Photographs are also a helpful insert to aid in explanation for family members who were unable to attend the consultation. I think there’s value in a tangible letter taken home to revisit.
Treatment letters are also an irreplaceable resource for my team. When a patient calls to schedule treatment previously presented, my stored letter immediately becomes a reference for scheduling appointments, including time allotments and space in-between subsequent visits. In my office, we offer a courtesy for treatment paid in full. This amount is figured in the financial investment portion of my letter so that conversations regarding immediate payment or a payment plan can easily flow. Should a case not be accepted prior to a routine recare visit, this letter serves as an excellent reminder during team huddle. It’s inefficient to page through multiple chart notes and software-driven plans with no explanation of the diagnoses which caused a need for restoration in the first place.
In my first few years of practice, it was hard for me to accept that I needed to view this document as fluid with a potential need for multiple modifications to suit my patient’s desires and limitations. For example, financial concerns often lead to the need for phased treatment or a compromise from the ideal. I’m committed to openly discussing what may occur if no treatment is rendered or if a compromised approach is chosen. Likewise, I believe in the importance of presenting the financial component of extensive treatment myself. As the dentist and business owner, I must “own” the fee that I’ve carefully determined to reflect indirect and direct time, the skill level and support to be provided by my team, the technical excellence of my laboratory technicians, and my own knowledge. The fee that I present is steadfast, barring an unanticipated need such as root canal therapy. Should there be a need for additional chair-time or visits, it’s included in the quoted fee.
Finally, my letters include my expectations for post-treatment maintenance. For example, if we are to complete a hybrid case in conjunction with a surgeon, I’m careful to share the importance of periodontal health and frequent maintenance visits to prevent peri-implantitis. In patients who have pre-existing medical conditions that when uncontrolled can be contradictory, I stress the importance of regular monitoring. Ultimately, I strive to empower my patients to choose and achieve oral health, Undoubtedly, oral health positively impacts overall health. My personal letters are a distinguishing trait of my practice that convey the level of care to be carried from presentation through treatment and in maintenance. Consider the value in this extra step!